Doppler ultrasound is a very handy tool in confirming the diagnosis of multiple medical conditions, and anyone using ultrasound in the ED should be familiar with its function and limitations.
There are three main modalities of Doppler in US: continuous wave, pulsed wave and color Doppler.
How does it work?
Not surprisingly, "Doppler" is named after its inventor, Johann Christian Doppler (1803-1853), an Austrian physicist. Doppler employs the principles of "The Doppler Effect" which is based on the change in frequency that is reflected back from red cells as they pass through a lumen or cavity (the heart).
The "Doppler Shift" refers to the equation Doppler Shift= (Fs - Ft), where Fs is the frequency of the scattered ultrasound beam after striking a moving object, and Ft is the frequency of the transmitted ultrasound beam. The reflected frequency will be higher when striking an object moving TOWARD a receiver (as in a fire truck coming towards you with a higher pitch) and lower when the object is moving away from a receiver.
Another slightly confusing equation that illustrates an important concept is the relationship between the Doppler Shift and blood flow velocity (V, in meters per second).
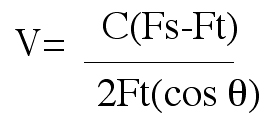
Notice that the bottom half of the equation includes the "cosine of theta," where theta equals the intercept angle between the ultrasound beam and the direction of blood flow. When this angle is parallel toward or away from the transducer (an angle of 0 deg or 180 deg), the result will be "1," which nullifies this value in the equation. However, if the cosine of 90 degrees is zero, meaning that if the beam is aimed directly perpendicular to blood flow, no Doppler Shift will result. For this reason,we always try to measure color and spectral Doppler parallel to blood flow (i.e. in the apical four chamber when assessing tricuspid and mitral valves).
So what happens when you're not measuring exactly at 0 degrees or 180 degrees? -- well lucky for us, a deviation from 0 or 180 by up to 20 degrees only produces an error in velocity calculation of 6%. Be careful though, a 60-degree intercept produces up to a 50% underestimation of velocity!
Flow coming towards the transducer will always be RED, while flow away from the transducer will be BLUE. A helpful mnemonic is BART (Blue away, Red towards).
Below is a video illustating color flow through the mitral valve of my heart:
Question: If I had a regurgitant jet, what color would it be?
Color off
Spectal Doppler Modalities (Continuous Wave Doppler and Pulse wave Doppler)
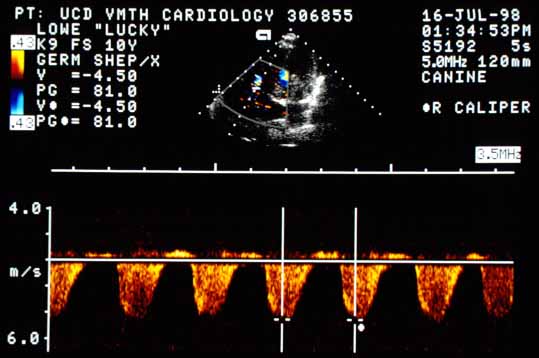
Most people are very familiar with color Doppler and its appearance on ultrasound. Spectral Doppler however, displays information in a slightly different manner. Continuous Wave doppler is commonly used in echocardiography for assessing velocity of blood flow in high flow rate states (i.e. stenotic valves); here, Pulsed Wave Doppler becomes inaccurate due to the high velocity of flow exceeding the Nyquist limit (out of the scope of this discussion). Two crystals are used in continuous wave doppler, (one sending crystal and one receiving crystal). The only downside regarding the continuous wave mode is that the sample area is through the entire length of the ultrasound beam (i.e. recordings from all signals within the beam are reported.) A Continuous Wave Doppler wave is "filled in" as compared to pulse wave doppler since it records lower-velocity signals proximal and distal to the point of maximum velocity, which fill in the waveform. In the ED we do not use continuous wave often.
Continuous wave doppler of tricuspid regurgitation (notice the waveform is below baseline)
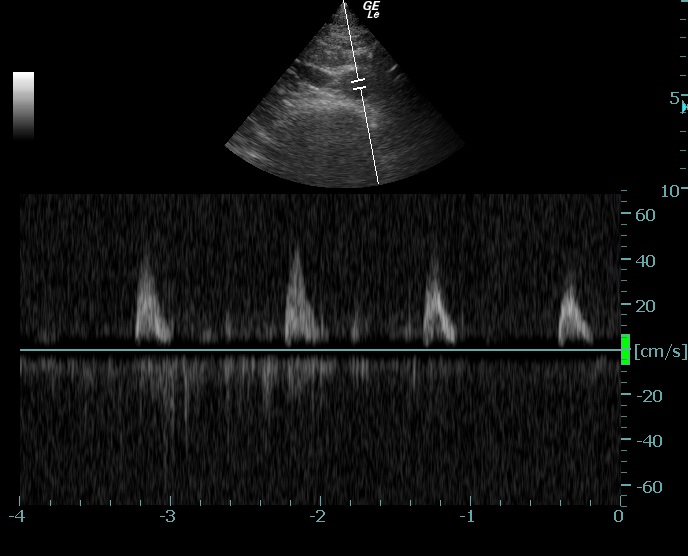
Pulse Wave Doppler however, is quite useful for ED applications. In this mode, velocity from a specific point can be measured. True to its name, a beam is "pulse" out of the transducer, and the same crystal which generated the beam then 'listens" for the return signal. A time interval between the "sending" phase is determined based on where the caliper was placed for sampling. The cycle of send, wait, and listen is determined by the Pulse Repetition Frequency which is measured in cycles/sec. Frequently, the reason why you may not be getting a "good" waveform on your spectral doppler analyses is because the PRF needs to be adjusted to allow for recording of lower flow rates. To do this, one would decrease the PRF. If you are receiving too large of a waveform to discern if it is artererial or venous on the screen, you should decrease the PRF.
An image of pulsed wave doppler mode showing an arterial "spike" waveform. X axis is time, while the Y axis is velocity in cm/sec.
I find spectral Doppler to be particularly helpful in obtaining an objective display of whether I'm looking at the abdominal aorta or the IVC in patients suspected of having a AAA.
Power Doppler mode and Aliasing
|