Discussion
The incidence of ectopic pregnancy has increased dramatically over the last thirty years to a current rate of around 2% of all pregnancies, however in the ED population, the prevalence may be as high as 13%. Fortunately, due to vigilance by ED physicians and better diagnostic techniques, maternal mortality due to ruptured ectopic has decreased, though it still remains the leading cause of maternal mortality in the first trimester and the second leading cause overall.
A classic triad for ectopic pregnancy has been identified and consists of abdominal pain, amenorrhea, and spotting or abnormal vaginal bleeding. Rarely do patients present with all three components of the classic triad, therefore any woman who presents with abdominal pain, syncope or signs of unexplained hypovolemia should have ectopic pregnancy considered in the differential diagnosis. Abdominal pain is the most common complaint in these patients and is present in up to 90%; amenorrhea varies from 40-70% and spotting in up to 80%.
Anything that causes damage to the fallopian tube may lead to an increased risk of ectopic pregnancy, but there are several major risk factors that are more consistently associated with ectopic pregnancies. These are pelvic inflammatory disease, tubal surgery, diethylstilbestrol exposure, use of an intrauterine device, assisted reproductive techniques, and prior ectopic pregnancy.
Physical exam signs may vary from subtle or nonexistent to very dramatic, but if a patient is pregnant, both transvaginal and transabdominal ultrasounds should be performed depending on dates of the pregnancy. If the UPT is negative then ectopic is less concerning, but the ultrasound is still useful for identifying ovarian/uterine cysts or masses or free fluid in the abdomen or pelvis from another source. If the UPT returns positive then a quantitative BhCG should be drawn to help determine whether or not the pregnancy may be visible by sonography. In many centers, TV ultrasound is performed first, and if an IUP is identified, the BHCG is deferred.
The BhCG level above which an intrauterine pregnancy should universally be visible by transvaginal sonography is known as the discriminatory zone. This value varies from institution to institution, but in ours has been set at 1500 mIU/mL. If the value is above this level, ultrasound either in the ED or performed by radiology should be able to determine the presence of an IUP if it indeed exists. If the ED is performing the US, remember, we are attempting to RULE IN an IUP, not rule out an ectopic. If you see anything other than an IUP defined by a CRL and or fetal pole within the uterus, additional workup and consultation will be necessary.
Many patients present to the ED with BhCG values less than 1500 mIU/mL. If after sonography the no IUP is seen and the mean gestational sac diameter is less than 20mm, the patient may either be discharged if stable to home and follow up with OBGYN in 48 hours for follow-up BhCG levels (certainly sooner for worsening symptoms). OB/GYN should be consulted if the patient has any signs of instability. Remember that BhCG levels should double every 48 hours during the first 6-8 weeks of pregnancy to a maximum of 100,000 mIU/mL. If a patient returns for 48 hour follow-up and the levels have increased at a slower than expected rate then ectopic should be suspected. Unfortunately some ectopic will rupture with HCG's less than 1500, as in our case presented here.
Flowsheet for First Trimester Vaginal Bleeding (discrim zone here is 1000 mIU/mL)

Treatment of the patient with ectopic pregnancy largely depends upon the stability of the patient and size of the pregnancy. Those with hemodynamic compromise may require emergent laparoscopy while those who are stable may be able to be treated as an outpatient. Those with lower BhCG levels (<10,000) may be candidates for methotrexate treatment with serial BhCG for monitoring efficacy.
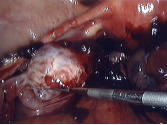
The patient's (blurry) intraoperative ectopic (thanks to OB for the image!)